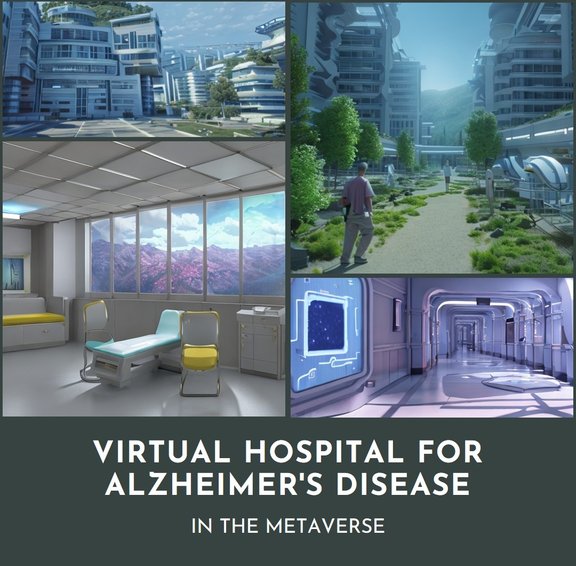
AlzCare Virtual Hospital for Alzheimer's Disease with a Virtual Digital Twin Patient...more precise and personalized treatments...
A Prof. specializing in Alzheimer's disease has a memory capacity of about 1.000 books...our Virtual Hospital has a memory capacity of 10-25 million books
.A neural symbolic LM can drastically improve diagnostic accuracy and reduce the number of misdiagnoses
Burden of serious harms from diagnostic error in the USA info@neuroteg.com
New drug for Alzheimer's disease Lecanemab ( Leqembi Biogen) versus IWP Light intensity running
Leqembi IWP
Side effects: infusion-related reactions, headache, allergic NO
Serious side effects: brain swelling, ARIA
Price: $26,500 /year + 12 x MRI scans about $12,000/y Price: 0
Numbers of Newly Born Hippocampal Neurons: X 1,7 more newly neurons
Not investigated?
Neural activity Hippocampus Test improved X 2
Beta-coefficient (Lure CR- Lure FA)
No hippocampus Test ? Why ??
Prefrontal cortex (attention and decision making) Reaction Time improved -50
No data? Why?
Hippocampus (memory responsible neurons) improved
No investigated? Why ?
BDNF Gene expression improved 150%
No investigated?
Japan: Prof Soya Hideaki Tsukuba University Medical Frontiers info@neuroteg.com
Context recognition - Emotional intelligence - domain expertise - neural symbolic reasoning ( combines neural networks and symbolic reasoning to solve complex problems )
Alzheimer's disease terminology is complex...clear prompts for doctors, caregivers or patients give you the best outcomes...ChatGPT alone cannot help you with clear prompts...
Creating a personalized ChatGPT for each patient that incorporates context recognition, emotional intelligence, and domain expertise can certainly help improve outcomes in healthcare settings. To get started, we will need to gather conversation data from each patient, as well as information about their individual preferences, interests, and health concerns. This data can be used to fine-tune a ChatGPT model that is tailored specifically to each patient's unique needs.
In terms of context recognition, the model can be trained to recognize different types of conversational cues and adjust its responses accordingly. For example, if a patient expresses concern about a specific symptom or side effect, the model can provide more targeted information and support to address that particular issue.
Emotional intelligence can be incorporated into the model by training it to recognize and respond appropriately to different emotional states, such as anxiety, sadness, or frustration. This can help the model provide more empathetic and supportive responses to patients, which can in turn help to build trust and rapport.
Finally, domain expertise can be integrated into the model by training it on relevant medical and healthcare information, such as common symptoms, treatment options, and medication side effects. This can help ensure that the model is providing accurate and reliable information to patients.
Overall, by incorporating context recognition, emotional intelligence, and domain expertise into personalized ChatGPT models for each patient, we can help to improve outcomes and provide more effective and tailored support to patients in healthcare settings
A ToM task is a type of psychological assessment used to measure an individual's ability to understand and attribute mental states, such as beliefs, desires, intentions, and emotions, to themselves and others, and to use this understanding to predict and explain behavior. ToM tasks are often used in the study of social cognition, developmental psychology, and neuropsychology.
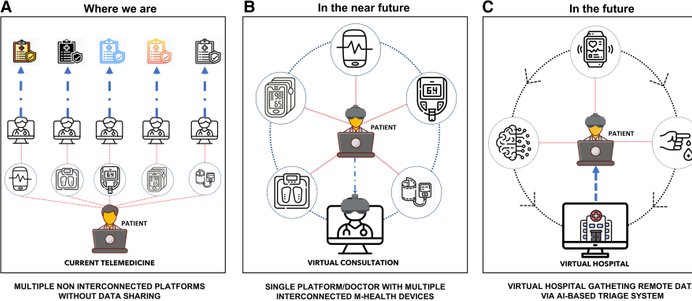
Democratizing the Metaverse and Virtual hospital for the elderly...without headset or glasses
Diffusion refers to the process by which particles move from an area of higher concentration to an area of lower concentration until an equilibrium is reached. Stable diffusion occurs when the process reaches a steady state where the concentration of particles remains constant over time. In a system with stable diffusion, the rate of diffusion is equal in all directions and the concentration gradient is maintained by a continuous supply of particles. This can occur in a variety of physical and chemical systems such as the diffusion of gases or solids in a medium. Stable diffusion is an important concept in many scientific fields, including physics, chemistry, and biology as it underlies many natural phenomena and processes, such as the exchange of oxygen, and carbon dioxide in the respiratory system, the movement of ions in a solution, and the diffusion of neurotransmitters in the brain.
Diffractive lightfield backlighting technology DLB
DLB technology is a type of display technology that uses a backlighting system to create a 3D visual effect on a 2D screen. The technology creates a 3D effect by using multiple layers of diffraction gratings, each layer controlling the light in a specific direction. As a result, the viewer's eye perceives different images from different angles, creating the illusion of depth. DLB technology has several advantages over other 3D display technologies. It is more efficient than other technologies because it does not require the use of additional panels or glasses to create the 3D effect. This means lower costs, and easier to use and maintain. Applications in medical imaging for creating 3D visualizations of the human body but also for the Metaverse for the elderly and virtual hospital...
Synthetic Methuselah fruit fly AI/Biolog hybrid model Synthetic Methuselah fruit fly Noch (N) gene
An Alzheimer's disease patient's digital twin is designed to capture continuous data from the individual about various vitals, medical condition, response to a treatment or drug and surrounding ecosystem. Unique digital twin from each patient help in determining right therapy, predict the outcome of a specific procedure and manage Alzheimer's disease.The Medicalverse shouldn't be a replacement for the real world. It should help you augment the real world. It should allow you to do things that maybe were not possible in the physical world.
AR is going to be more common than VR because it doesn't remove you from your physical reality. I can still be present in my physical world and that is important for Alzheimer's patients. We can train disrupted parts of the brain in a home environment...train disrupted neural circuits so that other circuits can take over the disruped function of this specific neural circuit.
Creating a personalized ChatGPT for each patient that incorporates context recognition, emotional intelligence, and domain expertise can certainly help improve outcomes in healthcare settings. To get started, we will need to gather conversation data from each patient, as well as information about their individual preferences, interests, and health concerns. This data can be used to fine-tune a ChatGPT model that is tailored specifically to each patient's unique needs.
In terms of context recognition, the model can be trained to recognize different types of conversational cues and adjust its responses accordingly. For example, if a patient expresses concern about a specific symptom or side effect, the model can provide more targeted information and support to address that particular issue.
Emotional intelligence can be incorporated into the model by training it to recognize and respond appropriately to different emotional states, such as anxiety, sadness, or frustration. This can help the model provide more empathetic and supportive responses to patients, which can in turn help to build trust and rapport.
Finally, domain expertise can be integrated into the model by training it on relevant medical and healthcare information, such as common symptoms, treatment options, and medication side effects. This can help ensure that the model is providing accurate and reliable information to patients.
Overall, by incorporating context recognition, emotional intelligence, and domain expertise into personalized ChatGPT models for each patient, we can help to improve outcomes and provide more effective and tailored support to patients in healthcare settings
AI chatbot for dementia and Alzheimer's patients
The robots that caregivers want
Un. of California San Diego
Study Alzheimer's and Dementia robots
- pet-like robots
- cleaning robots
- telepresence robots
- smart speakers
- wearables
1. Robots to be capable of facial recognition
2. Support positive moments shared by caregivers and their loved ones
3. Lessen caregivers emotional stress by taking on difficult tasks...such as answering repeated questions and restricting healthy food
4.Robots should be able to adopt to new situations ( progression of the disease)
5. Robots should be able to learn from end users and customize and personalize
6. Human-l with ike components not look like humans
7. Interact with human via voice activation
^Personality of our robots are based on the OCEAN personality theory
In 2011, a researcher did a postmortem analysis of 426 Japanese-American residents of Hawaii, about half of whom had been diagnosed with some form of dementia, typically Alzheimer’s. According to the autopsies, roughly half of that group had been misdiagnosed as having Alzheimer’s — their brains didn’t show evidence of the brain lesions typical of the disease. At a 2016 conference, Canadian scientists presented preliminary findings, based on more than 1,000 individuals, that patients were correctly diagnosed only 78 percent of the time. In nearly 11 percent of cases, patients thought to have Alzheimer’s actually didn’t, while another 11 percent did have the disease but weren’t diagnosed.
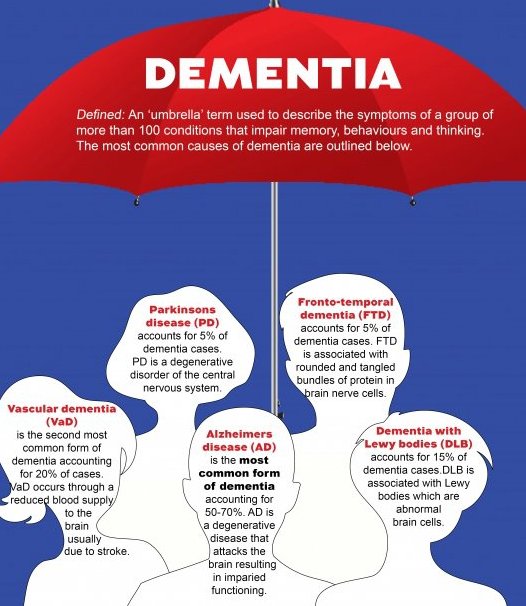
Accurate diagnosis is needed for Dementia Lewy Body
Dementia with Lewy Bodies (DLB) may account for up to 30% of all dementia cases. The symptoms of DBL can be difficult to disentangle from other dementia subtypes. DLB is characterized by a build-up of abnormal proteins (Lewy bodies) in areas that control cognition, movement, allertness and behavior.
Eye tracking ( saccadic eye movement tracking) and EEG are very sensitive digital biomarkers to make an accurate diagnosis.
AD and DLB pathologies often overlap within individuals. An individual is diagnosed with Parkinson disease dementia ( PDD) or DLB depends on the timing of symptoms onset. In dementia with Lewy Bodies, cognitive decline occurs within one year of the onset of movement disorder symptoms.
DLB is sensivity to antipsychotic drugs. We see also REM behavior disorder. Visual hallucinations and fluctuations in cognition, attention and allertness.
Mild Cognitive Impairment or MCI
MCI causes a slight but noticeable and measurable decline in cognitive abilities, including memory and thinking skills. Long-term studies suggest that 15-20 percent of the aged 65 and older may have MCI. There is a difference between normal aging cognitive decline and MCI. With all kind of rating scales it is not possible to see any difference.
Biomarkers for Alzheimer's disease can be really measured to indicate the presence or absense of the disease. For AD there is only one biomarker accepted amyloid beta. Preclinical b. amyloid as biomarker is difficult and very expensive to detect and it is only possible in hospitals. Digital biomarkers can be used outside the hospital POC ( in the waiting room or at home).
Blood glucose levels are a biomarker for diabetes and blood cholesterol for heart disease.
These are the most commonly misdiagnosed conditions.
Parkinson’s disease
It is a degenerative disorder of the central nervous system with symptoms including tremors in hands, arms or legs, stiff muscles, and problems with balance or walking.
However, it is commonly mistaken for Alzheimer’s disease, stroke, stress, a traumatic head injury and essential tremor.
Grave’s disease
The condition causes an overactive thyroid gland, and is the most common cause of hyperthyroidism.
Symptoms include eyes bulging, anxiety, sweating, rapid pulse, unplanned weight loss or gain, and extreme tiredness.
Without treatment, it can prove life-threatening, however it is often mistaken for depression, ageing and under-exercising.
Fibromyalgia
It is a chronic arthritis-like disorder characterised by widespread pain.
However, symptoms - anxiety, sensitivity to pain and incapacitating fatigue - can be confused with rheumatoid arthritis and chronic fatigue syndrome.
Normal pressure hydrocephalus
It is a build-up of cerebrospinal fluid in the brain that most commonly occurs after a stroke or ahead injury from a fall.
Symptoms of unsteady gait, progressive dementia and urinary problems, can be interpreted as Alzheimer’s disease or Parkinson’s disease.
Multiple Sclerosis
The progressive autoimmune disease that attacks the central nervous system has symptoms including muscle spasms, lack of coordination, balance problems, blurred vision and cognitive impairment.
However, it is commonly mistaken for a viral infection, lupus, Alzheimer’s disease and bipolar disorder.
Coeliac disease
It is an autoimmune disorder marked by an inability to digest gluten, a protein in wheat, rye and barley.
Symptoms can include vomiting, abdominal pain and bloating, diarrhoea, weight loss, anaemia and leg cramps.
However it can be mistaken for irritable bowel syndrome, Crohn’s disease and cystic fibrosis
Chronic fatigue syndrome
The complex disorder has no known cause but symptoms include loss of memory or concentration, a sore throat, painful lymph nodes in neck or armpits, unexplained muscle or joint pain and extreme exhaustion.
It is often confused with sinus problems, hepatitis, fibromyalgia, lupus and rheumatoid arthritis.
Lupus
It is a chronic inflammatory disease, with symptoms including fatigue, kidney, heart and lung damage, rash and joint pain.
However, it can be mistaken for chronic fatigue syndrome, fibromyalgia and rheumatoid arthritis.
Aortic dissection
This is where a tear develops in the aorta, the largest blood vessel branching from the heart, which causes the inner and middle layers to separate.
Symptoms can include sudden chest or upper back pain, loss of consciousness, shortness of breath, sweating and weak pulse in one arm.
However it can be misdiagnosed as heartburn, heart attack and stroke.